How Are People With Loss of Proprioception Able to Sit Up and Walk Again
Original Editor - The Open Physio project.
Top Contributors - Lucinda hampton, Admin, Kim Jackson, Amanda Ager, Vanessa Rhule, WikiSysop, Paule Morbois, Scott Buxton, Naomi O'Reilly, Tarina van der Stockt, Claire Knott, Amrita Patro, Wanda van Niekerk and Rachael Lowe
Page Owner - Amanda Ager as function of the Ane Folio Project
Introduction [edit | edit source]
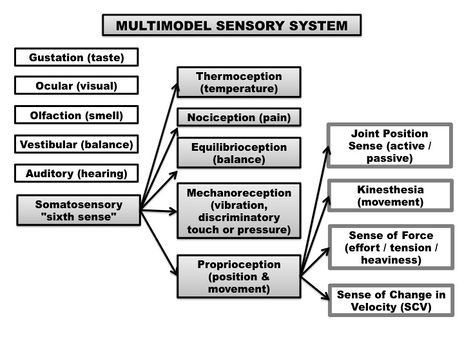
Proprioception (sense of proprioception) is an important bodily neuromuscular sense. It falls nether our "6th sense", more commonly known as somatosensation. The term somatosensation (or somatosensory senses) is an all encompassing term which includes the sub-categories of mechanoreception (vibration, force per unit area, discriminatory touch), thermoreception (temperature), nociception (pain), equilibrioception (remainder) and proprioception (sense of positioning and move).[i] The feedback from all these different sensory components arise from our peripheral nervous system (PNS), and feed information to our central nervous system (CNS), both at the level of the spinal string (reflexive) and sent to the cognitive cortex for college processing.[2]
Proprioception itself tin can exist understood as including various sub-modalities:
Proprioception (Articulation Position Sense): Proprioception is our sense of joint / limb positioning. It is often measured through articulation position sense - active joint position sense (AJPS) and passive joint position sense (PJPS). Joint position sense determines the ability of a person to perceive a presented joint angle and then, later on the limb has been moved, to actively or passively reproduces the same joint angle[iii] (Clinically measured equally a joint matching job).
Kinaesthesia: Kinaesthesia (kinaesthesis) is the awareness of motion of the human body (movement sense).[4] Sense of move refers to the ability to appreciate joint movement, including the elapsing, direction, aamplitude, speed, acceleration and timing of movements.[three]
Sense of Force: Sense of Force (SoF) is also known as sense of attempt / heaviness / tension or the force matching sense. It is the ability to reproduce (or lucifer) a desired level of strength one or more than times. Sense of forcefulness is thought to stem from the afferent feedback of the Golgi Tendon Organs (GTOs) embedded within our tendons, the musculus spindles within our muscles and proprioceptions within our peel.[five]
Sense of Change in Velocity (SoV): SoV is our ability to notice vibration, derived from oscillating objects placed against the pare.[6] It is believed to travel through the same type of large afferent nerve fibers (Aαβ) equally proprioception.[7]
Somatosensation. Retrieved from: Ager, A.L., Borms, D., Deschepper, L., Dhooghe, R., Dijkhuis, J., Roy, J.S., & Cools, A.Proprioception and shoulder hurting: A Systematic Review.J Paw Ther. 2019 Aug 31. pii: S0894-1130(nineteen)30094-viii. doi: 10.1016/j.jht.2019.06.002.
Globally, all sub-modalities of proprioception arise from the sum of neural inputs from the joint capsules, ligaments, muscles, tendons, and skin, in a multifaceted system, which influences beliefs regulation and motor control of the body.[8]
Proprioception is critical for meaningful interactions with our surrounding surroundings. Proprioception helps with the planing of movements, sport operation, playing a musical instrument and ultimately helping us avoid an injury.
The neurological basis of proprioception comes primarily from sensory receptors (mechanoreceptors and proprioceptors) located in your skin, joints, and muscles (muscle spindles with a smaller component from tendon organ afferents, cutaneous receptors and minimal input from articulation receptors). These muscle afferents receptors allow for the identification of limb position and movement via neural signalling of a change in musculus, skin or joint stretch[9]. Hence, proprioception is basically a continuous loop of feedforward and feedback inputs between sensory receptors throughout your body and your nervous system.
A mechanoreceptor is a sensory receptor in your torso that responds to mechanical changes of tissues. Different types of mechanoreceptors include
- Pacinian Corpuscles
- Meissner's Corpuscles
- Merkel's Discs
- Ruffini Corpuscles
- Golgi Tendon Organs (GTO)
- Free nervus endings
There are also mechanoreceptors within the hair and skin.
At that place are four types of mechanoreceptors found within ligamentous tissues. As all the types of mechanoreceptors are myelinated and rapidly transmit sensory information to the CNS.[10]
- Type I: (small) Depression threshold, slow adapting in both static and dynamic settings;
- Blazon II: (medium) Low threshold, apace adapting in dynamic settings;
- Type III: (big) High threshold, slowly adapting in dynamic settings;
- Type 4: (very pocket-sized) Loftier threshold pain receptors that communicate injury.
Type 2 and Type 3 mechanoreceptors in particular are believed to exist linked to one's sense of proprioception.[10]
The brusk video below gives a good insight into the complexities of proprioception.
[11]
Causes of Proprioception Damage [edit | edit source]
Poor proprioception at a joint may event in the increased likelihood of an injury.[12] The reason for proprioception impairments are not clear at this fourth dimension. A decreased sense of proprioception can be acquired by localized tissue impairment, the presence of edema (swelling) or competitive nociceptive inputs (presence off hurting).
Proprioception can exist affected by the following factors:
- Temporary impairment from a compromised land (for example the consumption of alcohol).
- Age-related changes besides affect proprioception. The run a risk of proprioception loss increases every bit nosotros age due to a combination of natural age-related changes to the nerves, joints, and muscles.
- Injuries or medical conditions that affect the neuromuscular system (muscles, nerves, and the cerebellum, CNS) which can cause long-term or permanent proprioception impairment.
Proprioception impairments have been noted among the following neurological conditions:
- Brain injuries; multiple sclerosis (MS); stroke; Parkinson's affliction; Huntington'southward disease; ALS (amyotrophic lateral sclerosis)
- Likewise health conditions: herniated disc; arthritis; autism spectrum disorder (ASD); diabetes; peripheral neuropathy.
- Post-surgery: joint replacement surgery, such every bit hip replacement or knee replacement
- MSK conditions: talocrural joint sprains, ACL injuries, shoulder dislocations and tendinopathies, whiplash associated disorders (among others).
Assessing Proprioception [edit | edit source]
The measurement of proprioception is presently non well adult. Proprioception can only be confidently measured in a laboratory setting, using complex figurer-interfaced equipment. At that place is before long a lack of valid, reliable and responsive tools and outcome measures to quantify proprioception deficits, in a clinical setting.[13]
If y'all suspect a proprioception deficit, focus on the post-obit clinical aspects.
Subjective assessment should include questions regarding the post-obit:
- Balance issues, such as having trouble standing on one foot or frequent falls while walking or sitting;
- Uncoordinated movement (ataxia), such equally not being able to walk in a straight line, or difficulty reaching for an object;
- The abstention of sure activities, such equally climbing stairs or walking on uneven surfaces because of a fear of falling.
Objective assessment should include observation of the above and the points below:
- Overal coordination (Reaching tests, Star Excurtion Balance Test, Upper extremity coordination tests);
- Awkwardness, such as dropping or bumping into things;
- Poor postural command, such every bit slouching or having to place extra weight on a tabular array for residual while sitting;
- Problem recognizing the appropriate level of muscular strength for a chore (for example: pressing on a pen too hard when writing or non being able to gauge the forcefulness needed to pick up an object).
There are a few clinical tests Physiotherapists tin can apply to assess proprioception, depending on the body office beingness assessed. The include:
- Romberg examination;
- Heel-shin. The patient is asked to bear on the heel of one foot to the contrary knee and and then to drag their heel in a straight line all the fashion downwardly the front of their shin and back up once again. In lodge to eliminate the effect of gravity in moving the heel down the shin, this examination should always be done in the supine position.
- Ataxia. Best revealed if the examiner'southward finger is held at the extreme of the patient's attain, and if the examiner's finger is occasionally moved suddenly to a different location.
- Finger—nose—finger test. The patient is asked to alternately touch on their nose and the examiner's finger as quickly every bit possible
- Distal proprioception examination. The tester will move the joints of the hip, knee ankle and big toe up and down while you watch. You then ask the client to echo the aforementioned motility with your eyes closed.
- A contralateral joint matching task. Asking the patient to match a demonstrated joint angle, and measuring the difference between the bodily joint angle, and the reproduced joint angle (the difference representing the proprioception error).
Learning New Skills [edit | edit source]
An intact sense of proprioception is crucial to learning a new skill. During the learning of any new skill, (sport performance or an artistic activity, for instance) it is normally necessary to go familiar with some proprioceptive tasks specific to that action. Without the appropriate integration of proprioceptive input, an artist would not be able to brush pigment onto a canvas without looking at the hand as it moved the brush over the canvas; it would be impossible to drive an machine because a motorist would not be able to steer or use the foot pedals while looking at the road alee. A person could not touch-type (typing without looking at the keys) or perform a ballet dance. The lesser line remains that our sense of proprioception is important to railroad train and develop, as it allows usa to interact with our environments without the dependence on visual feedback (for example, reaching for a cup on the summit shelve, without looking at the cup).
Physiotherapy - Training Proprioception [edit | edit source]
No matter the underlying crusade of a proprioceptive deficit, clinicians can rehabilitate patients with tasks and activities to improve motor skills, strength,balance and coordination. They can also aid patients learn how to manage daily tasks (ADLs) while living with a proprioception dysfunction.
There is converging evidence that proprioceptive preparation can yield meaningful improvements in somatosensory and sensorimotor function.[14] Retraining of a somatosensory function includes whatever interventions that addresses the remediation of the somatosensory modalities. Intervention methods include:
- Education;
- Repetitive do and feedback in detecting, localising, discriminating, or recognising different sensory stimuli, pressure, or objects; PRACTICE, Do, PRACTICE!
- Proprioceptive grooming;
- Remainder training (unstable surfaces, unpredictable situations with an external stimuli);
- Dual task training (in the absence of visual feedback for example)
- Somatosensory stimulation,[xv]
A 2019 review on sensory retraining of the leg post-obit a stroke, concluded that interventions used for retraining leg somatosensory impairment significantly improved somatosensory office and balance, but not gait suggesting a specificity of training effect.[15]
A 2005 systematic review of the effect of proprioceptive and residuum exercises on people with an injured or reconstructed anterior cruciate ligaments, reported that proprioceptive and residual exercise improves outcomes in individuals with ACL-deficient knees.[sixteen] Similarly a 2015 review on ankle sprains amongst a sporting population, ended that proprioceptive grooming programmes are effective at reducing the charge per unit of re-injury, particularly amidst those with a history of talocrural joint sprain.[17]
The effectiveness of physiotherapy treatment on remainder dysfunction and postural instability in persons with Parkinson'due south disease: a systematic review and meta-analysis in 2016 reported that physiotherapy interventions similar rest training combined with muscle strengthening, range of movement and walking training exercise is effective in improving balance in patients with Parkinson's disease. As proprioception can also be improved with balance grooming, this could possibly advocate for proprioceptive retraining every bit well, amongst this population.[18]
Proprioception rehabilitation often include: [edit | edit source]
-
ane. Balance exercises. Continuing on a Balance board is ofttimes used to retrain or increment proprioception abilities, particularly equally physical therapy for ankle or knee injuries. You can as well perform weight bearing exercises on an unstable surface (such as a Bosu Ball or stability disc) for the upper extremities (such every bit push ups, or simply weight bearing on elbows or an outstretched arm position).
2. Tai Chi, which improves lower limb proprioception and Yoga, which improves balance and muscle strength. The slow, focused movements of Tai Chi practice provide an environment whereby the proprioceptive information being fed back to the brain stimulates an intense, dynamic "listening surroundings" to further enhance mind / body integration.
3. somatosensory stimulation preparation, such as vibration therapy, dissimilar textures (cotton fiber ball vs. velcro);
4. Joint repositioning training (joint matching tasks).
For complimentary topics, please read the post-obit pages:
Neuromuscular Exercise Plan
Coordination Exercises
Developmental Coordination Disorder and Concrete Activity
Sensorimotor Impairment in Neck Pain
References [edit | edit source]
- ↑ Ager, A.L., Borms, D., Deschepper, 50., Dhooghe, R., Dijkhuis, J., Roy, J.S., & Cools, A.Proprioception and shoulder pain: A Systematic Review.J Mitt Ther. 2019 Aug 31. pii: S0894-1130(xix)30094-8. doi: x.1016/j.jht.2019.06.002.
- ↑ Guyton Air-conditioning. Textbook of Medical Physiology. 8th ed. Philadelphia, PA WB Saunders; 1992.
- ↑ 3.0 3.1 Riemann, B. L., & Lephart, S.1000. (2002). The sensorimotor arrangement, part 1: the physiological basis of functional joint stability. Journal of Athletic Training, 37(ane),71-79.
- ↑ Sherrington CS. On the proprio-ceptive system, especially in its reflex aspect. Brain. 1907;29:467–482.
- ↑ Hung, Y. J. (2015). Neuromuscular control and rehabilitation of the unstable ankle.World Journal of Orthopedics,half-dozen(v), page 434.
- ↑ Gilman, S.,Joint position sense and vibration sense: anatomical arrangement and assessment.Periodical of neurology, neurosurgery, and psychiatry, 2002.73(v): p. 473-7.
- ↑ Shakoor, North., A. Agrawal, and J.A. Block,Reduced lower extremity vibratory perception in osteoarthritis of the articulatio genus.Arthritis and rheumatism, 2008.59(one): p. 117-21.
- ↑ Blanche, E.I., Bodison, South., Chang, G.C., & Reinoso, G. (2012). Development of the Comprehensive Observations of Proprioception (COP): Validity, Reliability, and Factor Analysis. Am J Occup Ther. 66(6): 691–698. doi:x.5014/ajot.2012.003608.
- ↑ Suetterlin KJ, Sayer AA. Proprioception: where are nosotros at present? A commentary on clinical assessment, changes across the life class, functional implications and future interventions. Age and ageing. 2013 Nov 14;43(3):313-8. Bachelor from: https://academic.oup.com/ageing/article/43/3/313/16765 (last accessed 31.x.19)
- ↑ ten.0 10.1 Michelson JD, Hutchins C. (1995). Mechanoreceptors in human ankle ligaments.The Periodical of Bone and Articulation Surgery. British Volume.77 (2): 219–24. PMID 7706334.
- ↑ W Deloriea Proprioceptors Available from: https://www.youtube.com/watch?v=Dzlkz8j-8rg ( concluding accessed 30.ten.2019)
- ↑ Anderson, V. B., & Wee, E. (2011). Impaired joint proprioception at higher shoulder elevations in chronic rotator cuff pathology. Arch Phys Med Rehabil, 92(vii), 1146-1151. doi:10.1016/j.apmr.2011.02.004
- ↑ Ager, A.Fifty.,Roy, J.Due south., Roos, M., Belley, A.F., Cools, A., & Hebert, L.J. (2017). Shoulder proprioception: How is it measured and is it reliable? A systematic review.J Paw Ther.,30(2), 221-231. doi: ten.1016/j.jht.2017.05.003.
- ↑ Aman JE, Elangovan Northward, Yeh I, Konczak J. The effectiveness of proprioceptive preparation for improving motor function: a systematic review. Frontiers in human neuroscience. 2015 January 28;8:1075. Bachelor from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4309156/ (last accessed 31.10.2019)
- ↑ 15.0 fifteen.1 Chia FS, Kuys S, Low Choy Northward. Sensory retraining of the leg afterwards stroke: systematic review and meta-analysis. Clinical rehabilitation. 2019 Jun;33(6):964-79. Available from: https://journals.sagepub.com/doi/total/ten.1177/0269215519836461 (terminal accessed 31.x,2019)
- ↑ Cooper RL, Taylor NF, Feller JA. A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed inductive cruciate ligament. Research in sports medicine. 2005 Apr 1;xiii(2):163-78. Available from: https://www.tandfonline.com/doi/total/10.1080/15438620590956197 (last accessed 31.10.2019)
- ↑ Schiftan GS, Ross LA, Hahne AJ. The effectiveness of proprioceptive grooming in preventing talocrural joint sprains in sporting populations: a systematic review and meta-analysis. Journal of Scientific discipline and Medicine in Sport. 2015 May 1;18(3):238-44. Available from: https://www.jsams.org/article/S1440-2440(14)00074-7/fulltext (concluding accessed 31.ten.2019)
- ↑ Yitayeh A, Teshome A. The effectiveness of physiotherapy treatment on residue dysfunction and postural instability in persons with Parkinson's disease: a systematic review and meta-assay. BMC sports science, medicine and rehabilitation. 2016 Dec;viii(i):17. Bachelor from: https://bmcsportsscimedrehabil.biomedcentral.com/manufactures/ten.1186/s13102-016-0042-0 (last accessed 31.10.2019)
luciasustoespen1936.blogspot.com
Source: https://www.physio-pedia.com/Proprioception
0 Response to "How Are People With Loss of Proprioception Able to Sit Up and Walk Again"
Publicar un comentario